Over 95% of the country is metabolically inflexible, and insulin resistance is a causal driver, with hypertension a frequent comorbidity. In July 2022, a study1 in the Journal of the American College of Cardiology from Tufts showed that 14 out 15 Americans, over 93% of the population, are metabolically inflexible, and insulin resistance and blood pressure are two of the key parameters of metabolic fitness.
Current statistics are likely even worse. The study used data from 2018, prior to the pandemic, which radically worsened metabolic health. So, in all likelihood, well over 95%, or 19 out of 20 people, are metabolically unfit. Excessive salt intake has long been accused of causing high blood pressure, and reducing salt intake typically does result in an initial reduction in blood pressure.
In one November 2023 study,2,3 reducing salt intake by 1 teaspoon a day (which equates to 2.3 grams of sodium) reduced systolic blood pressure by an average of 6 to 8 millimeters of mercury (mm Hg) in 75% of participants in a single week — a result comparable to taking blood pressure medication. But is that all there is to it? Hardly.
Is Salt Intake Really the Problem?
According to conventional thought, salt induces high blood pressure by making your body absorb more water.4 Excess sodium in your blood absorbs water, thereby increasing the amount of blood filling up your vessels. As a result, your heart must work harder, hence your blood pressure goes up.
However, lowering your sodium intake isn’t the answer here. As detailed in “Trashing the Eight Glasses of Water a Day Recommendation,” while reducing salt intake may initially lower your blood pressure, it comes at a cost. In the long run, it worsens dehydration and ultimately results in higher blood pressure.
This occurs because when your salt intake is very low, your body responds to the decrease in blood volume by preventing your kidneys from excreting sodium. By retaining sodium, it helps increase your blood volume. It also increases vasoconstriction (narrowing of the blood vessels) to bring the blood pressure back up.
And, by forcing your kidneys to retain sodium, they will excrete potassium and magnesium instead. These are the primary intracellular electrolytes required for cellular hydration. Low magnesium and potassium also leads to further vasoconstriction and increased sympathetic nervous system activity.
Your sympathetic nervous system is the gas pedal that speeds up the systems involved in the fight-or-flight response, so it causes stress. Norepinephrine is also released when sodium levels are low, which also fuels the stress response. The stress response, in turn, ratchets up blood pressure. So, in the long run, too little salt can promote high blood pressure.
Electrolyte Imbalance Can Affect Your Blood Pressure
Oftentimes, a deficiency in the other electrolytes (calcium, potassium and magnesium) are part of the problem. Your sodium-to-potassium ratio is particularly important for healthy blood pressure.
Potassium helps lower your blood pressure by relaxing the walls of your arteries, and according to Harvard Health,5 many people with high systolic blood pressure can successfully lower it simply by increasing their potassium intake.
Prior to 2019, the adequate intake (AI) for potassium was 4,700 mg per day, based on the median intakes in healthy people. In 2019, the daily recommended intake was reduced to 2,600 mg a day for women aged 19 and older, and 3,400 mg a day for men, 19 and older.6
It is likely the higher 4,700 mg a day recommendation is the wiser one, and it’s generally recommended that you eat five times more potassium than sodium. If you’re unsure of your sodium and potassium intake, use cronometer.com/mercola. This nutrient tracker allows you to enter foods and then calculates the ratios automatically.
In my view the best way to increase your potassium is by eating ripe fruit. I typically get around 3,000 mg from watermelon, orange juice, apples and tangerines, and another 2,000 mg from other sources.
For a more complete list of potassium-rich foods, see DietaryGuidelines.gov’s “Food Sources of Potassium” page.7 Taking potassium supplements is not a good strategy and simply will not provide you with the benefits you seek. Magnesium also plays a significant role in the modulation of blood pressure, so you do not want to be deficient in that either.
Estrogen — A Wholly Overlooked Factor in High Blood Pressure
According to the late Ray Peat, a biologist and physiologist who specialized in the bioenergetic theory of health,8 estrogen is a major factor in the development of hypertension.
He believed there is a strong relationship between estrogen, nitric oxide (NO) and carbon dioxide (CO2). He explained that while estrogen promotes the production of NO, a gas that can help lower blood pressure by relaxing your blood vessels. NO also binds to complex IV and impairs mitochondrial energy production and increased insulin resistance.
Estrogen also interferes with your body’s ability to produce CO2, another gas that is essential for oxygen transport. As a result, high estrogen can result in low blood oxygen levels, which can contribute to high blood pressure.
Estrogen can also interfere with your body’s production of progesterone, a hormone that helps maintain normal blood pressure by regulating your blood sugar level and reducing inflammation. Progesterone is also an estrogen antagonist, which is important because estrogen, like linoleic acid (LA), draws water inside the cell, which increases blood pressure.
So, salt is hardly the only thing that causes water retention and swelling. Both estrogen and LA, which most processed foods are loaded with, do this as well.
If your blood pressure is high, and especially if your salt intake is already within reasonable limits, you’d be wise to assess whether your estrogen level might be too high (especially if you’re on estrogen therapy, which I do not recommend), and/or if you’re consuming too much LA.
Anything over 10 grams of LA a day can cause severe problems. I recommend keeping your LA intake below 5 grams a day. Cronometer.com/mercola is a helpful tool here as well.
Normalizing Your Blood Pressure With CO2
Peat advised treating high blood pressure with exogenous (supplemental) CO2, as it’s your body’s primary vasodilator. NO is a secondary “emergency” vasodilator. A simple way to do this is to take one-half to three-quarters of a teaspoon of baking soda in water a few times per day.
You can also boost your CO2 level by breathing into a paper lunch bag for a minute or two. The bag should not be too small or too large (an ideal size is 6 inches by 15 inches, or 15 centimeters by 38 centimeters). Breathe into the bag with your mouth and nose covered. Other exogenous delivery strategies include:
- Drinking carbonated water and other carbonated beverages
- Improving dysfunctional breathing habits
- Nasal cannula administration
- Rectal insufflation — This was the preferred administration method in the 1800s and 1900s. A 1-liter bag or 1-quart bag filled with CO2 gas, attached to a rectal catheter is used here; and it’s something that is relatively easy to do at home, provided you have the right equipment
If you are going to use CO2 therapeutically, make sure you’re getting beverage grade CO2. Beverage grade is 10 times cleaner and purer than food grade, and it’s the kind used in restaurants. You do not want industrial grade, which is used for cryo chambers, welding and a variety of other typically commercial applications.
Commercially, beverage grade CO2 is typically sold or rented in 20-pound cylinders. There’s enough CO2 gas in one cylinder that if you’re using 1 liter a day therapeutically, it will last you 250 years.
There are smaller units, like SodaStream, that can provide CO2 gas. The problem is that you need to use those CO2 cylinders with SodaStream equipment, and there is no easy way to put the gas into a container or bag, so you can’t use those cylinders for insufflation. A SodaStream is the ideal choice if you’re making carbonated beverages, however.
How Insulin Influences Your Blood Pressure
Insulin resistance is also a major contributor to high blood pressure, and one of its main causes is excess LA in your tissues. Additionally, your kidneys produce hormones that regulate arterial and venous constriction and your circulating blood volume. These two functions work together to maintain your blood pressure within normal limits.
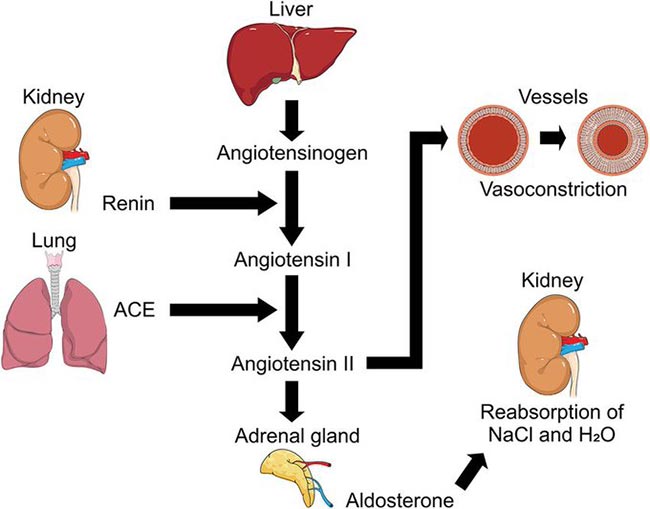
Within your kidneys are special cells responsible for sensing the amount of sodium in the filtrate, and others that sense your blood pressure. As your blood pressure drops, the amount of filtered sodium also drops. In response to this drop in sodium, these specialized kidney cells release an enzyme called renin.
Renin, in turn, is converted into angiotensin I, and then to angiotensin II, a peptide hormone that causes vasoconstriction and an increase in blood pressure. At the same time, angiotensin II stimulates the adrenal gland to secrete aldosterone, an adrenal hormone that controls the amount of water your kidneys retain.
It does this by stimulating reabsorption of sodium, which pulls more water with it. The increase in sodium and water reabsorption then reduces your urine output and increases your circulating blood volume. Both of these functions affect your blood pressure measurements.
However, aldosterone is also activated by elevated insulin. So the increase in blood volume is not really an excess sodium problem per se. The problem is that too much sodium is being retained due to excess insulin.
Indeed, the class of blood pressure medications known as ACE inhibitors lower blood pressure by blocking the conversion of angiotensin. As a result, less aldosterone is produced, less sodium is reabsorbed, and less water is retained. Angiotensin II blockers also block this hormone directly.
So, to summarize, insulin resistance — which results from eating a diet too high in LA — is a major contributor to high blood pressure because elevated insulin leads to sodium retention, which draws in water and increases your blood volume, thereby raising your blood pressure. The graph below, posted on Twitter/X by the Mind Muscle Project,9 illustrates this sequence.
Key Strategies to Normalize Your Blood Pressure
In closing, here is a list of some of the key lifestyle strategies to help normalize your insulin sensitivity and blood pressure:
Limit your LA consumption to 5 grams a day or less — Excessive omega-6/LA consumption contributes to high blood pressure by increasing mitochondrial dysfunction by several mechanisms that we will not review here. The easiest way to do this is to ditch all processed foods (as they all are likely loaded with LA), and focus on a diet of whole foods, ideally organic. It would be helpful to also eliminate seeds and nuts unless you have been on a low LA diet for at least three years. Sources of healthy fats to add to your diet include: grass fed butter, raw organic dairy, organic pastured egg yolks, coconuts, coconut oil and macadamia nuts, grass fed meats and pasture-raised poultry. The best carbs to add would be ripe fruit that you tolerate well. Just make sure your fat intake is below 30%, which you can determine with Cronometer. If you fail to do this the carbs can convert to fat and change your cholesterol profile unfavorably. |
Optimize your vitamin D, as vitamin D deficiency appears to be associated with both arterial stiffness and hypertension.10 |
Optimize your sodium-to-potassium ratio, and make sure you’re getting enough magnesium and calcium as well. |
Exercise regularly — Exercise is well-known for its ability to normalize blood pressure, but all forms of exercise are not the same in this regard. A recent investigation revealed that isometric exercise, where your muscles are in static contraction, is the most effective for lowering blood pressure, while aerobic exercise is next to last in terms of effectiveness.11 |
Avoid estrogen therapy, and never take estrogen without progesterone. |
Consider using some form of exogenous CO2 supplement. |
