November 14, 2018
Pneumococcal exposure and colonization have been shown to elicit immune responses that may be beneficial in later life.
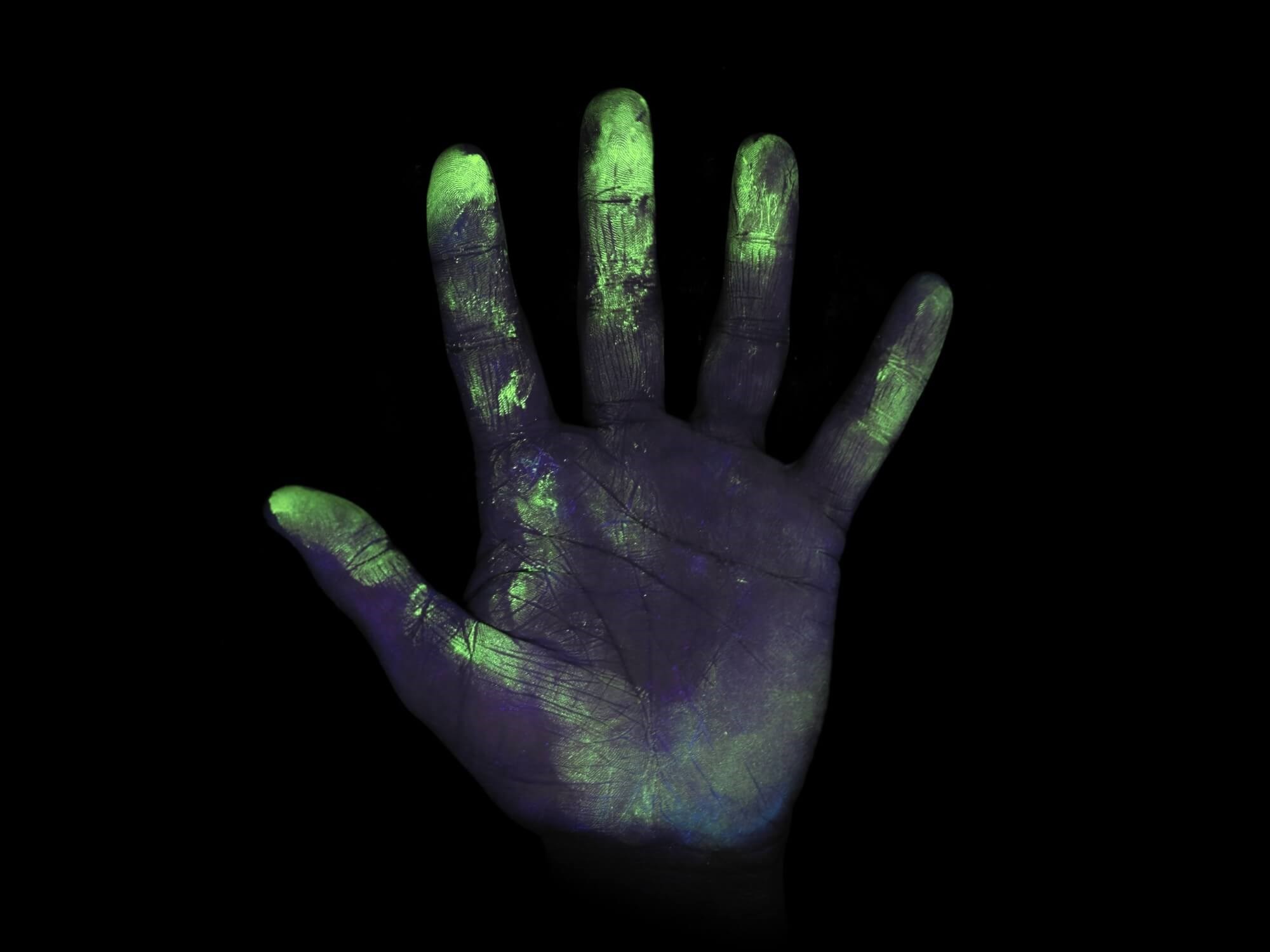
Hands can be vehicles for transmission of pneumococcus and lead to acquisition of nasopharyngeal colonization, according to research published in the European Respiratory Journal.
Streptococcus pneumoniae (pneumococcus) is a major cause of acute otitis media, sinusitis, pneumonia, and meningitis worldwide, with more than 1.2 million attributed deaths annually. Colonization of the nasopharynx with these bacteria is a prerequisite for infection and it is the primary reservoir for transmission. It is theorized that transmission of pneumococcus occurs primarily through indirect contact through inhalation of airborne droplets and is associated with living in higher-density populations. For upper respiratory tract infections in general, direct contact is implicated in disease transmission, which can be interrupted by hand washing. However, the relative contribution of direct and indirect transmission modes to pneumococcal colonization and disease are unknown. Therefore, this study sought to assess the potential for pneumococcal hand-to-nose transmission to cause nasopharyngeal colonization.
A total of 63 healthy adult participants were enrolled into a controlled Experimental Pneumococcal Challenge model that was modified to assess “hand-to-nose” (ISRCTN identifier: 12909224). Participants were divided into 4 transmission groups and administered pneumococcus (3.2X106 mid-log phase colony-forming units of S pneumoniae serotype 6B) onto their hand and asked to either sniff or make direct contact with the nasal mucosal surface with the bacterial residue either immediately after exposure (wet) or when visibly dry (1-2 minutes after exposure). The 4 groups were: (1) sniffing wet bacterial suspension (wet sniff), (2) sniffing bacterial suspension after air-drying (dry sniff), (3) pick/poke nose with finger exposed to wet bacterial suspension (wet poke), and (4) pick/poke nose with finger exposed to bacterial suspension after air-drying (dry poke). After 9 days of exposure, nasopharyngeal colonization was assessed through nasal washes and all samples were tested by quantitative polymerase chain reaction (qPCR) with primers for lytA and for S pneumoniae serotype 6A/b.
Of the 40 participants, 20% were found by culture at follow up to be experimentally colonized with pneumococcus (6B), with the highest rates in the wet poke (40%) and wet sniff (30%) groups. In the dry sniff and dry poke groups, 10% and 0% of participants, respectively, were found to be experimentally colonized. When wet and dry groups were compared, colonization rates in the wet groups were significantly higher than in the dry groups (P =.04, Fisher exact test). Molecular detection via lytA qPCR identified higher colonization rates compared with culture (P <.0001). This was most apparent in the dry poke group, which had a colonization rate of 0% by culture and 70% using qPCR. Samples that were only positive with qPCR, such as the dry poke group, tended to have lower densities of carriage compared with samples that were positive with both methods, such as both of the wet groups.
Overall, the results provide a better understanding of the duration of survival of pneumococci in nasal secretions on the hands and the entire transmission process. The study authors concluded that, “This modification of the Experimental Pneumococcal Challenge model has several potential uses, including testing of current or new hand cleaning interventions to ensure reduction in transmission of this important bacterial pathogen.”
Reference
Connor V, German E, Pojar S, et al. Hands are vehicles for transmission of Streptococcus pneumoniae in novel controlled human infection study. Eur Respir J. 2018;52(4):1800599.
